Wisdom Tooth Removal in Mooresville
What Are Wisdom Teeth?
Wisdom teeth, also referred to as third molars, are the last teeth to develop. They are located in the back of your mouth on both the top and bottom jaw. Wisdom teeth usually erupt into the oral cavity around 15-17 years of age, complete eruption around 20 years old, and complete their development by age 23. Many times, there is insufficient room in your mouth for the proper eruption and function of your wisdom teeth, and they are considered impacted. This can lead to future problems, including pain, infection, cavities, or bone loss on adjacent teeth.
When Should You Remove Your Wisdom Teeth?
Your oral surgeon or dentist will recommend the removal of your wisdom teeth in your teenage years to help prevent these future problems. In fact, it is recommended that wisdom teeth be removed when the roots are ½-⅔ formed, usually by age 17. In some cases, your teeth may have developed faster than expected, and wisdom tooth removal may be recommended as early as 12 years old. Having wisdom teeth removed early not only prevents future problems from arising but also allows for quicker healing and easier recovery.
Reasons for Wisdom Tooth Removal
Prevention of root resorption – Impacted wisdom teeth can exert enough pressure on the adjacent tooth that it can lead to the resorption, or breakdown, of the roots on the adjacent tooth. Removing impacted wisdom teeth early can prevent the loss of adjacent teeth due to root resorption.
Prevention or treatment of periodontal disease (bone loss) – The teeth adjacent to impacted wisdom teeth have an increased risk of developing periodontal disease or bone loss. Impacted wisdom teeth pushing against the back side of the teeth in front of them (the second molars) decreases the amount of bone on the back side of the second molars. This area is also very difficult to keep clean, which allows the accumulation of food and bacteria, which leads to inflammation and further bone loss.
If impacted wisdom teeth are removed before the age of 25, there is better and more complete regeneration or healing of the bone levels on the back side of the second molars. If impacted wisdom teeth are left in place, it is more likely for significant bone loss to develop on the adjacent teeth, increasing the risk they will also require extraction. Extracting the wisdom teeth will help prevent further bone loss on adjacent teeth.
Pericoronitis – When there is insufficient space in the mouth for complete eruption of the wisdom teeth, they often only partially erupt. This may cause the soft tissue (gum tissue) that is partially covering the wisdom teeth to become inflamed and infected. The opposing teeth can also cause trauma to this inflamed gum tissue causing further swelling and discomfort. If left untreated, this localized infection can spread to deeper tissues and cause a more serious infection. Removing wisdom teeth can prevent pericoronitis from forming and treat pericoronitis if it has developed.
Pathology – During development, all teeth are contained within a dental follicle which is a sac-like structure that the tooth is surrounded by. As teeth erupt, the follicle is broken down. When a tooth is impacted, the dental follicle is usually retained. Over time the follicle may undergo cystic changes, become larger, and develop into a cyst. If left untreated, cysts can continue to grow and cause the destruction of adjacent bony structures and teeth. Removing wisdom teeth early can help prevent the development of these cysts.
Caries (cavities) – When wisdom teeth are malpositioned or impacted, it makes cleaning the area on the distal, or back side, of the second molars more difficult. Again, this allows cavity-causing bacteria to accumulate and often allows cavities to form on the distal of the second molars. Often the cavity forms close to the level of the bone, making restoration difficult or impossible. These teeth usually will require extraction. Removing wisdom teeth early creates an environment that is more cleansable, decreasing the risk of cavities forming on second molars. Additionally, food and bacteria often accumulate under the gingival tissues that partially cover partially impacted wisdom teeth. This area is again difficult to clean and increases the risk of cavities and infection in the wisdom teeth themselves.
Orthodontic treatment – With cases of crowding, your orthodontist may need more space to allow the movement of other teeth. Impacted wisdom teeth may require removal to allow for these movements to be made. Otherwise, the impacted wisdom teeth may prevent proper movement of other teeth during orthodontic treatment. Sometimes impacted wisdom teeth may prevent the eruption of your second molars, which normally erupt around age 12. In these cases, it may be necessary to remove your wisdom teeth at an earlier age to allow for proper eruption of your second molars.
Levels of Impaction:
Erupted / not impacted – This is when wisdom teeth have fully emerged from the gum tissue. Often, they erupt in an abnormal position or angulation, making them difficult to care for and clean.
Soft tissue impacted – When the wisdom teeth are partially covered in gum tissue, this often leads to inflammation and pain in the area as well as infection (pericoronitis).
Partial bony impacted – The wisdom tooth is partially covered in bone and gum tissue due to inadequate space for eruption. It is usually the distal, or back side, of the wisdom tooth that is covered in bone. The teeth are not in the correct position, are difficult to clean, and cannot function in chewing.
Complete bony impacted – The tooth is not present in the mouth and over ½ of the tooth is still covered in bone. The tooth may be minimally visible. There is no space for the tooth to erupt and function. This usually requires more complex removal techniques.
Unusually difficult complete bony impactions – The tooth has not erupted and is located in an unusual position that makes removal more difficult. This requires more complex removal techniques than normally required.
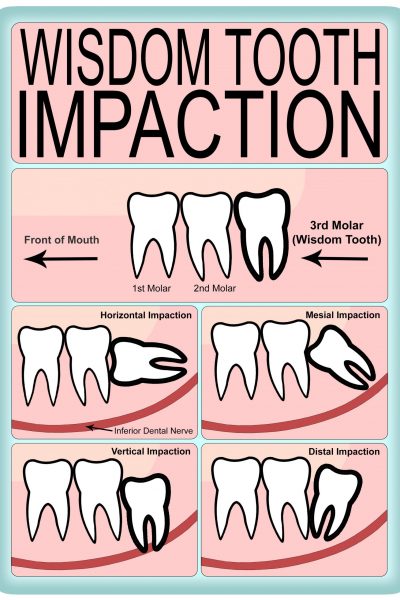
Additionally, wisdom teeth may also be classified based on their angulation.
Vertical impaction – The tooth is upright in a near normal orientation, just below the gum line and bone level.
Horizontal impaction – The wisdom tooth is sideways or “lying down.” The biting surface of the tooth is against the back side of the tooth in front of it.
Mesioangular – The tooth is tilted towards the front of the mouth. It often appears to be leaning over and “stuck” under the tooth in front of it.
Distoangular – The tooth is tilted towards the back of the mouth or away from the tooth in front of it. It appears to be tilting into the back of the lower jawbone. This usually requires more complex removal techniques.
How Are Wisdom Teeth Removed?
Wisdom tooth removal is best to be completed by a trained oral and maxillofacial surgeon. As oral surgeons, we have spent a minimum of 4 years of advanced training beyond dental school in areas that include implant placement, removal of impacted teeth, treatment of facial fractures, treatment of oral pathology, reconstructive jaw surgery, anesthesia, and cosmetic facial surgery. This training ensures that the surgeon performing your wisdom teeth extractions will do so in a safe and effective manner that will make for a simpler surgery, quicker and easier recovery, and a safer and more comfortable experience.
Wisdom tooth removal is usually completed under IV sedation/general anesthesia. This means that you will be sleeping during your surgery. Many patients prefer this method as they do not want to be aware of the surgery. It is possible to have wisdom teeth extracted with just local anesthesia (numbing medication). Your surgeon will talk to you about your options to help you decide which option is best for you.
What to Expect During Your Wisdom Tooth Extraction
If performed under general anesthesia, you will have an IV placed to allow for the administration of anesthesia. Additionally, you will have monitors attached that continually monitor your breathing, blood pressure, oxygen saturation, heart rate, and heart rhythm. These monitors are the same monitors used in hospital settings during the administration of anesthesia. This is all done to ensure optimal safety during surgery.
You will be administered oxygen through a nasal cannula throughout the surgery to ensure oxygen levels are maintained. However, you will not be intubated during this surgery as you will be breathing on your own throughout the procedure.
The procedure will take about 30-45 minutes, although this may differ based on individual cases. However, your total time at the office may be 1-1.5 hours to allow for adequate recovery from anesthesia.
What to Expect After Your Wisdom Tooth Procedure
It is normal to feel drowsy and sometimes nauseous after the procedure. This is from the anesthetic medications administered during surgery. It is recommended you go home and rest. Light meals such as crackers, applesauce, and ginger ale may help resolve post-op nausea.
You will still be numb after surgery due to the local anesthetics (numbing medication) administered. This is normal and will last for a few hours. This also allows you to get home and begin taking Ibuprofen and/or Tylenol before pain begins to set in.
It is recommended that you rest and “take it easy” for at least 2-3 days after surgery to allow for recovery. Do not engage in vigorous or strenuous physical activity, as this can increase the amount of discomfort and bleeding after surgery.
You may have sutures at the surgical sites. These are self-dissolving unless your surgeon informs you otherwise. The sutures usually will dissolve before the surgical sites are fully closed; this is normal.
It may take a few weeks for the extraction sites to close fully with gum tissue. This is because it takes a few weeks for the edges of the gum tissue to fully grow over and close the areas where the teeth were removed.
Pain is expected after the removal of wisdom teeth. Your surgeon will discuss post-operative pain expectations as well as medications used to manage your post-operative pain. It is recommended that you start with a combination of Ibuprofen and Acetaminophen (unless informed otherwise due to medical conditions or allergies) to help with your pain. Ibuprofen not only provides pain relief but helps with inflammation as well. Your surgeon may have prescribed opioid-based pain medications to be used as needed for severe pain for the first few days after surgery.
Swelling after surgery is a normal response your body has after surgical procedures. As your body begins to heal after surgery, an influx of cells and mediators facilitates healing. This will cause swelling at the surgical sites. Swelling usually peaks around 48-72 hours after surgery. Applying cold compresses, such as ice packs, bags of frozen vegetables, etc., to the outside of your face after surgery will help with pain and swelling. Apply cold compresses for 20 minutes, then keep them off for 20 minutes. If swelling worsens after 3 days and/or is accompanied by fevers/chills or drainage from the surgical sites, this is a sign of possible infection, and you should contact our office.
It is normal to have slight bleeding from the surgical sites for the rest of the day. Gauze is placed over the sites for you to bite on and place pressure to help stop post-operative bleeding. Extra gauze will be supplied; you should change the gauze with fresh gauze every 30 minutes. Ensure to wash your hands before changing gauze. If light bleeding persists, you may bite on a moistened tea bag for 30 minutes. Once the bleeding stops or has decreased to the point that it is not noticeable, you may stop biting on gauze. If there are any concerns regarding the bleeding, you are encouraged to call our office.
Eat a soft diet as there may be pain when chewing after surgery. You may feel a tightness in your jaw muscles that makes it difficult to open your mouth fully for a few days after surgery. This is a normal response due to inflammation around the jaw muscles in response to surgery.
Risks Following a Wisdom Tooth Extraction
Infection – Although rare, an infection can occur after any surgery, including tooth extraction. Signs of infection include worsening swelling, fevers/chills, drainage of white or yellow fluid from the site (pus), warmth at the site, and difficulty fully opening your mouth due to pain or tightness in the jaw. If you are experiencing these symptoms, you are encouraged to call our office, and we will schedule you for evaluation and treatment if needed. Treatment of a post-operative infection includes cleaning out/flushing the site to clean out debris and bacteria, draining any abscess that has formed, and administering antibiotics. Antibiotics may be prescribed as well as given through an IV in the office.
To help prevent infection, you are encouraged to keep the surgical sites clean by doing warm salt water rinses after meals or at least twice a day. You should also continue normal oral hygiene by brushing and flossing other teeth. We recommend not using over-the-counter mouth rinses as they may cause discomfort at the surgical sites.
Bruising – Light bruising to the outside of the face around your cheeks may occur. This is a normal response to surgery and will resolve with time. Applying cold compresses for the first 48-72 hours and then warm compresses afterward may help decrease the amount of bruising.
Dry socket (Alveolar osteitis) – When teeth are removed, a blood clot will form and fill in the hole where the tooth was removed. This blood clot plays a critical role in allowing healing to occur. If the blood clot is prematurely lost, there will be an empty socket where the tooth was extracted. This will cause inflammation of the bone at the extraction site and intense pain. This pain often radiates along the entire side of the jaw, into the ear, and along other teeth in the same area. Often, prescribed pain medications will not control this pain. Other symptoms that may occur are a bad smell or taste in your mouth. People who smoke and/or use birth control pills are at an increased risk of developing dry sockets, and it is more common in the lower jaw than in the upper jaw.
To help avoid developing a dry socket, you should rest for 48 hours after surgery, keep sites clean with gentle warm salt water rinses, and avoid mechanical debridement of extraction sites with objects like toothpicks or water picks. If you believe you have developed a dry socket, please call our office for a same-day appointment to treat the issue. Treatment consists of flushing bacteria and food debris out of the socket and applying a medicated dressing to the empty socket to relieve your pain. These medicated dressings only alleviate pain and do not aid in healing. The dressing may be replaced more than once if needed.
Prolonged numbness – Impacted lower wisdom teeth can come into close contact with the main nerve that supplies feeling to the lip, chin, teeth, tongue, and gum tissue. Sometimes with the removal of impacted wisdom teeth, there can be irritation of this nerve or injury to the nerve that results in prolonged numbness to the lower lip, chin, and tongue. This is usually a temporary numbness that resolves on its own within a few days, weeks, or months.
Complete recovery is both more likely to occur and to occur faster in younger patients. Additionally, nerve injury is more likely to occur in older patients when roots are fully formed and come in close contact with the nerve. This is another reason why extraction of impacted wisdom teeth is recommended in your teenage years.
Sinus communication – Upper wisdom teeth often come close to the floor of the maxillary sinus, a large air-filled space in your maxilla (top jaw). This bone is thin and delicate, and an opening may form when wisdom teeth (or other molars in the top jaw) are removed. If this occurs, an initial closure of the sinus will be completed at the time of surgery. This may result in sinus congestion or a slight nosebleed for the first few days after surgery. Your surgeon will inform you of this result and will give you instructions to decrease side effects and improve healing. In rare cases, you may require additional minor surgery to close the sinus opening if the initial closure does not obtain complete closure of perforation.
When Is a Good Time to Have a Wisdom Tooth Extraction if I Decide to Do it?
It is recommended to have the procedure performed when it will not interfere with school, work, sports, or other life events. Popular times are during summer and winter breaks from school. Additionally, most patients will only require 2-3 days of recovery before returning to work or school with little interference with normal activities. Really, wisdom tooth surgery can be performed at any time, and it is the patient’s decision on when is best to schedule.
For more information, you can go to https://myoms.org/what-we-do/wisdom-teeth-management/.